General Considerations
- Abnormal amount of fluid in the pericardial space, defined as the space between the visceral and parietal layers of the pericardium
- Normally contains about 20-50 cc of fluid
- Fat covers outside of heart and outside of pericardium sandwiching pericardial space between the two layers
- Normal thickness of pericardium (parietal pericardium and fluid in space) is 2-4 m
Clinical Findings
- Small effusions frequently produce no symptoms
- Chest pain or discomfort with a characteristic of being relieved by sitting up or leaning forward and worsened in the supine position\
- Syncope
- Palpitations
- Shortness of breath, tachypnea
- Muffled or distant heart sounds, tachycardia
- Hypotension
- Jugular venous distension
- Pulsus paradoxus
- Decrease in systolic pressure with inspiration of more than 10 mm Hg
- Rate of accumulation of fluid is proportional to severity of symptoms
- The faster the fluid accumulates, the more severe the symptoms
- Requires about 150-250cc before cardiac tamponade occurs
- About 7-10% of those with pericardial effusion are at risk for developing tamponade
- Tamponade compresses heart and causes low cardiac output
- Most effusions do not lead to cardiac tamponade
- Size of cardiac silhouette is frequently increased
- Tamponade is rarely seen in association with pulmonary edema in the lungs
Causes
Causes of Pericardial Effusions
|
Cause
|
Remarks
|
Myocardial infarction
|
Most common
|
Collagen vascular disease
|
Especially Lupus
|
Trauma
|
Surgical or accidental
|
Metastatic disease
|
Serosanguinous effusion
|
Tuberculosis
|
Uncommon except in AIDS
|
Viral infection
|
Coxsackie A and B virus
|
Uremia
|
18% in acute uremia
|
- Other causes
- Serous fluid or transudate
- Congestive heart failure
- Hypoalbuminemia
- Irradiation
- Blood (hemopericardium)
- Rupture of ascending aorta or pulmonary trunk
- Coagulopathy
- Fibrin (produces exudate)
- Pyogenic infection, e.g. staph
- Uremia
- More common in chronic renal disease than acute
Imaging findings
- Conventional radiography
- Suggestive but not usually diagnostic
- "Water bottle configuration" is symmetrically enlarged cardiac silhouette
- Major DDX is cardiomegaly
- Loss of retrosternal clear space
- Non-specific and frequently not valid
- "Fat-pad sign"
- Produced by separation of retrosternal from epicardial fat line >2 mm
- Rapidly enlarging cardiac silhouette with normal pulmonary vascularity
- Echocardiogram
- Study of choice
- Echo-free fluid between the visceral and parietal pericardium
- Early effusions accumulate posteriorly first
- > 1cm is usually defined as a “large” effusion
- CT
- May detect small effusions (50cc)
- Fluid-filled space surrounding the myocardium
- Early effusions accumulate posteriorly first
Treatment
- Medical treatment depends on cause and may include
- Non-steroidal anti-inflammatory agents
- Colchicine
- Steroids
- Antibiotics
- Chemotherapeutic agents
- Pericardiocentesis
- Pericardial sclerosis for recurring effusions
- Tetracycline, doxycycline, 5-fluorouracil
- Pericardial window
- Video-assisted thoracic surgery (VATS)
- Allows for wide resection of pericardium
|
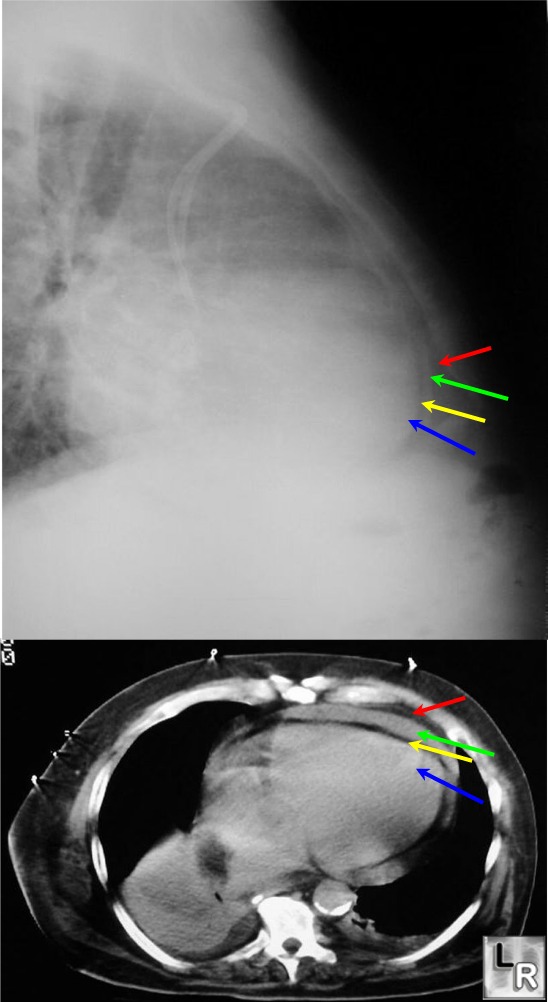
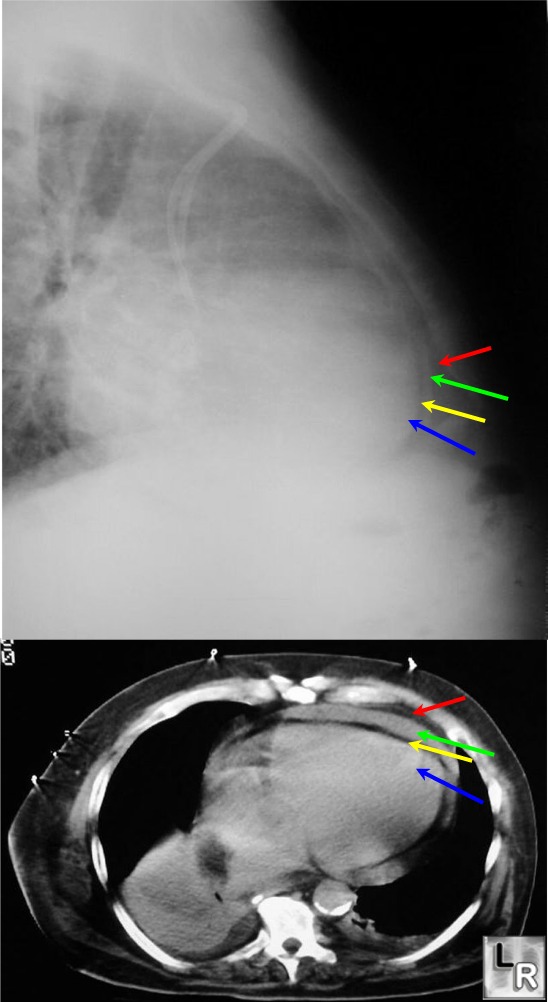
Pericardial effusion on both frontal chest radiograph and axial CT. Red arrow points to fat outside of pericardium. Green arrow points to pericardial space which is 8 mm in this patient (<4 mm is normal.) The yellow arrow points to fat outside of heart and the blue arrow to the myocardium.
retrieved from:http://www.learningradiology.com/archives04/COW%20112-Pericardial%20effusion/percardeffuscorrect.htm
No comments:
Post a Comment